MEET AIEOP’S WORKING GROUPS!
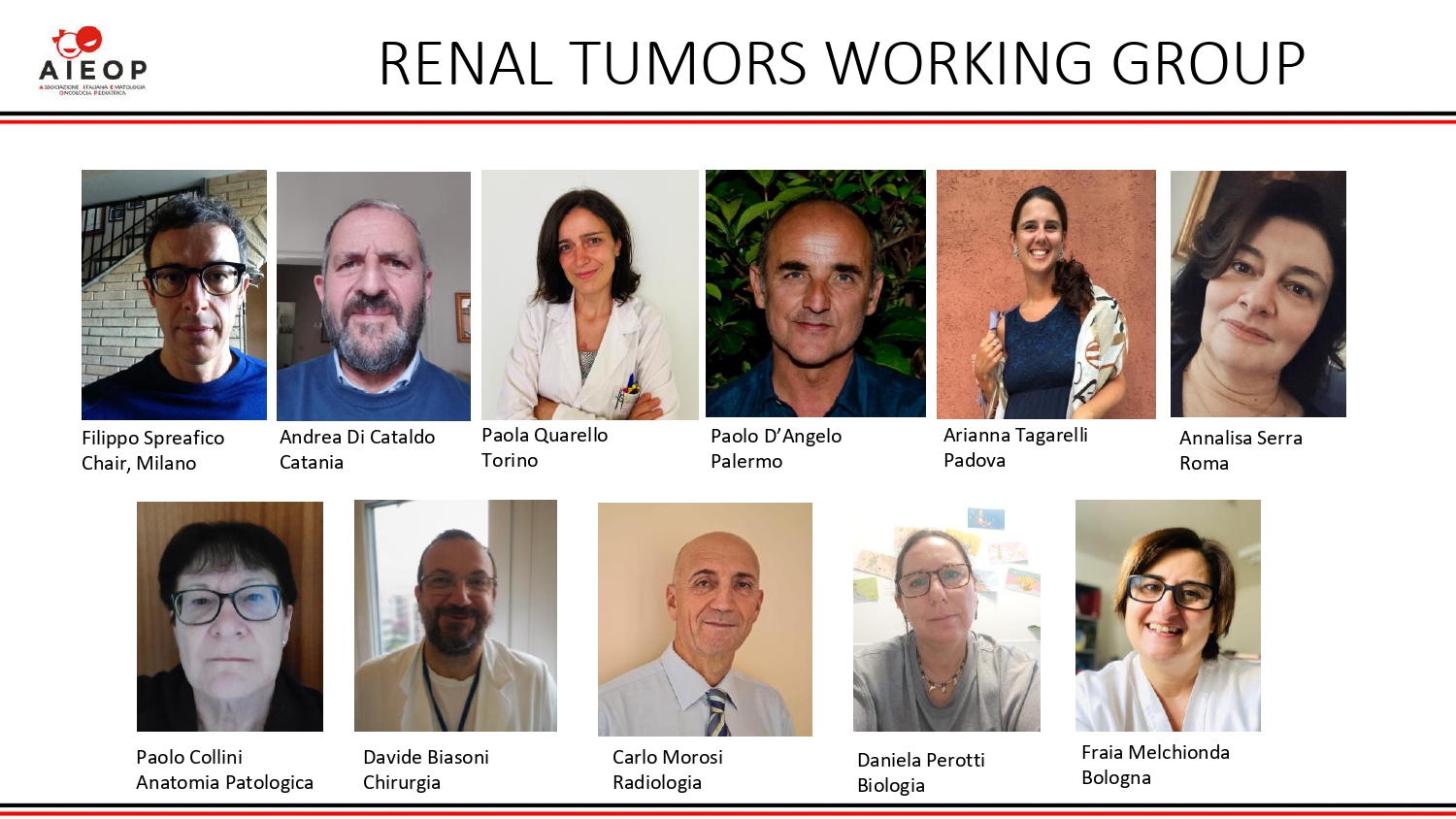
Meet the Renal Tumors Working Group
&
Coordinator Filippo Spreafico
Tell us a little bit about your background as Coordinator of the Working Group?
More than 25 years of practicing in a leading pediatric oncology unit have given me an exceptional opportunity to gain intensive education in oncology and pediatric oncology, and networking. This experience has included the fields of translational research, international outreach, and the development of clinical trials.
Over the years, the growing interaction with many AIEOP colleagues on renal tumors, translated in bringing these tumors the major focus of my clinical and research interest. Being then actively involved in the most intense professional network for pediatric renal tumors –i.e. SIOP Renal Tumor Study Group, I benefit from exchanging knowledge with the leading experts in this field around the world, including colleagues from the Children’s Oncology Group Renal Rumor Committee. This collaboration has recently given me the chance to lead a relevant educational global effort concerning renal tumors, resulting in a publication by the prestigious Journal Nature Review Disease Primers, which aimed at describing the current and most up-to-date standard of research and care for Wilms tumor.
My contribution to the international SIOP Renal Tumor Study Group, commenced as national coordinator for Italy, has significantly improved, leading the Relapse/Refractory renal tumor committee and becoming the elected Secretary General of the SIOP Renal Tumor Study Group Association in early 2022.
What is the overall goal and in addition a specific current goal of the WG?
Decades of clinical and basic research have helped to optimize clinical care for children with Wilms tumor, the most common pediatric renal tumor. Yet, 20% of patients with Wilms tumor relapse after first-line therapy, and the current treatment approach to non-Wilms renal tumor is less satisfactory. Ongoing prognostic classification for children with Wilms tumor is grounded in clinical and pathological findings and in only a few dedicated protocols on molecular alterations. A major goal is to introduce biology-driven approaches to patient risk stratification and new drug development, which has been slower in renal tumors than in other childhood tumors. Advanced imaging to capture tumor composition, optimizing irradiation techniques to reduce target volumes, and evaluation of newer surgical procedures are relevant areas for future research.
We should approach these goals on an internationally based cooperation, and with synergistic efforts given the limited resources.
What has been your WG’s greatest accomplishment?
I consider two achievements in the recent history of this Working Group as central ones. Thanks to the multidisciplinary collaboration of many experts and participation of almost all AIEOP centers, we were able to run and complete the national AIEOP-TW-2003 protocol, which was the first of a generation of modern studies for the cure of children with renal tumor in Italy, implementing centralization, sharing of complex cases, and investigating molecular findings as additional personalized prognostic signatures. Results of AIEOP-TW-2003 have been internationally shared through publications and meetings.
Also thanks to this coordinated effort, we are able to interact with SIOP Renal Tumor Study Group as a well-organized national Group. An historical gain (this is the second key achievement) was the official engagement with the SIOP Renal Tumor Study Group around 2010, becoming active members of this international networking, and joining the ongoing SIOP protocols for pediatric renal tumors for the first time.
What message do you have to the international medical community?
Curative therapy is achievable in 90% of children with Wilms tumor, yet striking survival disparities still exist within countries and between different parts of the world, which remain to be addressed and deserve commitment to change. Survival in low-income and middle-income countries is much lower than in high-income regions. This inequality also pertains to European regions. In 2020, WHO shared the Global Initiative for Childhood Cancer, designed to provide guidance to member states for the implementation of childhood cancer services in resource-constrained settings. Six tracer cancers, including Wilms tumor, are targeted to provide guidance for diagnosis, therapy and supportive and survivorship care. With the help of international pediatric cancer partners (academic, regional and global societies and non-governmental organizations), the aim is to establish the necessary training and design of basic, and translational and clinical research. Progress in Wilms tumor survival rates is expected to become more visible in the current decade.
Twenty percent of patients with Wilms tumor relapse after first-line therapy and up to 25% of survivors report severe late morbidity of treatment. Addressing the long-term effect of radical nephrectomy on renal function and cardiovascular function will probably drive more attention on expanding the role of nephron-sparing surgery.
Molecular studies are expanding the landscape of cancer genes implicated in Wilms tumor. The use of next-generation integrative genomic and epigenetic tumor analysis has provided important insights into Wilms tumor biology. Comparisons of the regulation of progenitor cells in the fetal kidney with the disrupted regulation of their counterparts in Wilms tumor should provide further insights into tumor formation. Targeting Wilms tumor genes with a non-redundant role in nephrogenesis and targeting the fetal renal transcriptome warrant further therapeutic exploration. Interventions that could prevent the evolution of nephrogenic rests to malignant Wilms tumor could transform therapy in this setting and could even lead to preventive strategies in children known to have disease susceptibility.

